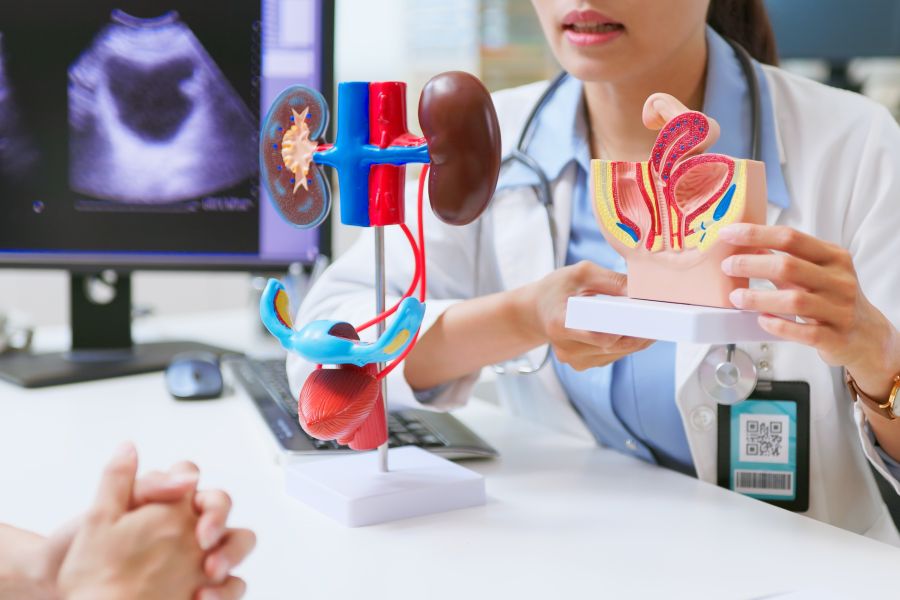
When it comes to women’s health, the bladder is often overlooked — until it becomes a problem. As a urogynecologist, I regularly see patients who have struggled in silence with issues like urinary incontinence, bladder prolapse and chronic urgency. These are common conditions, but they are not inherent to aging and are treatable.
What does the bladder do?
The bladder plays a vital role in the urinary system. It acts as a reservoir, storing urine produced by the kidneys until it is emptied from the body. A healthy bladder fills and empties with minimal effort or awareness. However, when the bladder isn’t functioning correctly, it can significantly impact quality of life.
Signs of an unhealthy bladder
Some of the most common signs of bladder dysfunction include:
- Urinary leakage during laughing, coughing, sneezing, or physical activity (stress incontinence)
- Urgency and frequency, with or without leakage (urge incontinence)
- A feeling of incomplete emptying
- Pressure or a bulging sensation in the vagina
- The need to manually adjust the position to empty the bladder fully
In some cases, women may experience continuous leakage following pelvic surgery, which may indicate a complication that requires further evaluation.
Understanding prolapse
Bladder prolapse, or cystocele, occurs when the bladder drops into the vaginal canal due to weakening of pelvic support structures. This can cause pressure, discomfort and visible or palpable bulging. Common risk factors include:
- Vaginal childbirth
- Aging and menopause
- Smoking (due to chronic coughing)
- Obesity
- Chronic constipation
- Repetitive heavy lifting
What Is incontinence?
Urinary incontinence is the involuntary leakage of urine and can be caused by multiple factors, including:
- Weak pelvic floor muscles
- Changes from childbirth
- Age-related changes to pelvic support
- Anatomical abnormalities or complications from prior surgeries
- Neurological conditions
Incontinence is not just a nuisance; it can affect sleep, confidence, intimacy and physical activity.
Prevention and self-care
Many bladder issues can be managed or prevented with simple lifestyle changes:
- Maintain a healthy weight.
- Avoid constipation by eating a fiber-rich diet and staying hydrated.
- Limit bladder irritants, such as caffeine, carbonated drinks, artificial sweeteners and acidic beverages.
- Practice pelvic floor exercises (Kegels) daily. I tell patients: “100 Kegels a day keeps the urogynecologist away.”
Kegels strengthen the muscles that support the bladder and urethra and are one of the most effective non-surgical tools in preventing or reducing symptoms.
Treatment options
If symptoms persist, don’t wait. Urogynecologists are specialists trained in both female pelvic medicine and reconstructive surgery. We offer comprehensive treatment options, including:
- Pessary devices: Non-surgical support placed in the vagina to relieve prolapse symptoms
- Minimally invasive surgery: Performed vaginally or laparoscopically with robotic assistance to restore pelvic support
- Behavioral and medication therapies for bladder control
The earlier these conditions are evaluated, the more options women have, often avoiding more extensive procedures down the road.
Final thoughts
You don’t have to live with bladder issues. They are common, but they are not normal — and they are certainly not something you should be embarrassed to talk about. At Northside Hospital, we are here to help you take charge of your pelvic health with expert, compassionate care.
Learn more about the Northside Center for Urogynecology.

