
Extracorporeal membrane oxygenation, or ECMO, is a powerful tool in the treatment of patients with severe cardiogenic shock and cardiac arrest. At Northside Hospital, specialists emphasize that while ECMO can be lifesaving, its success depends heavily on careful patient selection and responsible use.
Allison Dupont, MD, FSCAI, FACC, director of the Critical Care Unit and ECMO Program with the Northside Hospital system, recently highlighted the importance of balancing hope, hype and data when evaluating patients for veno-arterial (VA) ECMO.
“ECMO is an extremely resource-intensive therapy,” Dupont said. “Using it appropriately is critical to improving survival while avoiding unnecessary harm.”
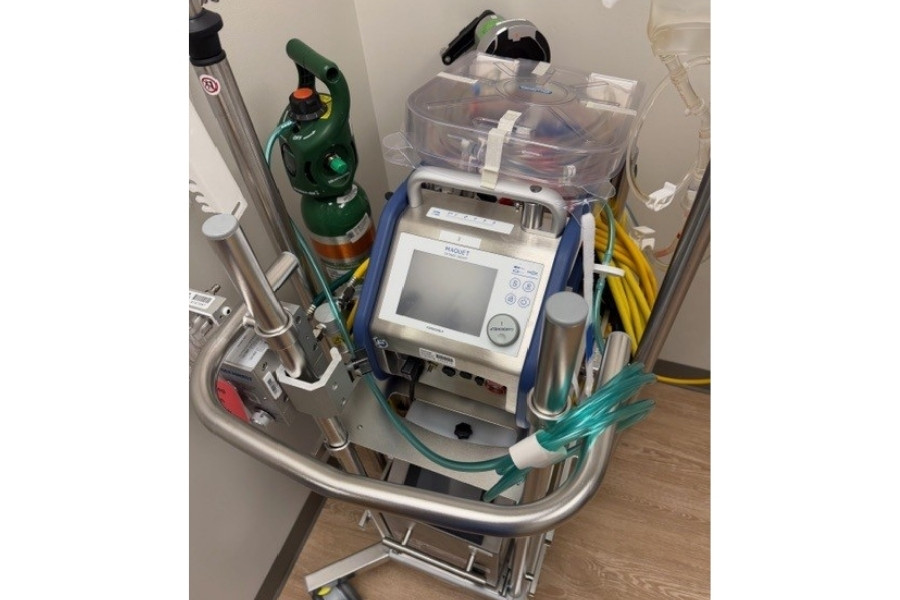
VA ECMO temporarily supports heart and lung function by circulating oxygenated blood throughout the body when the heart is unable to pump effectively. At Northside, ECMO is used as part of a comprehensive, multidisciplinary approach to treating complex cardiovascular emergencies, including cardiogenic shock and refractory cardiac arrest.
Limited randomized evidence
Despite increased use nationwide, there are currently no randomized clinical trials that definitively support routine VA ECMO use in cardiogenic shock. As a result, Northside clinicians rely on clinical expertise, registry data and patient-specific indicators when determining whether ECMO is appropriate. For example, patients with cardiogenic shock and evidence of ongoing organ hypoperfusion despite conventional therapies may be considered for VA ECMO.
When ECMO may not be appropriate
Northside physicians carefully evaluate each case to determine whether ECMO offers meaningful benefit. Relative contraindications include multiorgan failure, terminal malignancy or other end-stage disease, irreversible neurologic injury, and patients who are unlikely to recover native heart function but are not candidates for heart transplant or durable mechanical support.
Additional factors include prolonged cardiopulmonary resuscitation without bystander CPR, recent or expanding intracranial hemorrhage, hemorrhagic shock, and refusal of blood products. In these situations, ECMO may not improve outcomes and can prolong suffering.
ECMO during cardiac arrest
ECMO may also be used during extracorporeal cardiopulmonary resuscitation, or ECPR, for select patients with refractory cardiac arrest. At Northside, ECPR is considered for patients who meet specific criteria shown to be associated with better outcomes.
Patients most likely to benefit include those with a witnessed cardiac arrest, an initial shockable rhythm, and less than 10 minutes of downtime without CPR. Timing is critical, with ECMO ideally initiated within 60 minutes of the initial arrest. Younger patients generally experience better outcomes than older patients.
Additional physiologic markers may guide decisions, including arterial oxygen levels greater than 50 mm Hg, lactate levels of 18 mmol/L or lower, and end-tidal carbon dioxide levels above 10 mm Hg during resuscitation.
Identifying patients unlikely to benefit
Patients with unwitnessed cardiac arrest, nonshockable initial rhythms, prolonged downtime, extended delays to ECMO initiation, or severe chronic medical conditions are less likely to benefit from ECPR. Data from the Extracorporeal Life Support Organization registry further reinforce the importance of careful selection.
Commitment to responsible care
At Northside Hospital, ECMO is integrated into a coordinated system of cardiovascular and critical care services designed to deliver the right therapy to the right patient at the right time.
“ECMO can be lifesaving when used appropriately,” Dupont said. “Our goal is to ensure that every patient receives care that aligns with the best available evidence and their individual clinical situation.”
As ECMO technology and experience continue to evolve, Northside Hospital remains committed to advancing high-quality care for patients facing the most critical cardiac emergencies.
LEARN MORE ABOUT NORTHSIDE HOSPITAL HEART INSTITUTE.

